Cervical Cancer
İçindekiler
- 1 What is Cervical Cancer?
- 2 Major Risk Factors for Cervical Cancer:
- 3 What are the Symptoms of Cervical Cancer?
- 4 How is Cervical Cancer Diagnosed?
- 5 Cervical Cancer Treatment:
- 6 What are the Ways of Protection from Cervical Cancer?
- 7 Is Cervical Cancer Contagious?
- 8 False Information and Truths About Cervical Cancer (Cervical Cancer)
The cervix is the area where the top of the vagina meets the lower part of the uterus (womb). Cancers occurring in this area, namely cervical cancer (cervix), are one of the leading causes of cancer deaths in women all over the world. While 350 thousand new cases are detected every year in developing countries, this number is less than one hundred thousand in developed countries. This is due to the lack of effective screening programs in developing countries that aim to detect and treat cervical lesions before they progress to invasive cancer, that is, in the preinvasive period.
Early diagnosis of cervical cancer is of great importance for women’s health in our country where there is no effective and widespread screening program.
Thanks to the pap smear test, which detects precancerous changes in the cervix, death rates from cervical cancer have decreased by 50-70% in the last 50 years.
What is Cervical Cancer?

The cervix is the part of the lowest part of the uterus that connects to the vagina.
Cervical cancer occurs when cells of the cervix grow abnormally and invade other tissues and organs of the body. When this cancer is invasive, it affects the deeper tissues of the cervix and may spread (metastasize) to other parts of the body, particularly the lungs, liver, bladder, vagina, and rectum.
However, cervical cancer progresses slowly, so when we detect precancerous (pre-cancerous) changes, it is possible to detect, treat and prevent the progression of cancer early.
Most women diagnosed with precancerous changes in the cervix are in their 20s to 30s, but the average age of women at the time of being diagnosed with cervical cancer is in their mid-50s. This difference between the ages at which precancerous changes are most frequently diagnosed and cancer is diagnosed highlights the importance of slow progression of the disease and its prevention when adequate controls are made.
Cancerous changes begin at the squamocolumnar junction and there are changes in the cervical epithelium over the years, which is important in the early diagnosis of cervical cancer.
These changes are:
Normal endocervical columnar epithelium —> Squamous metaplasia —> Mild-moderate-severe dysplasia —> Carsinoma in situ —> Microinvasive carcinoma —> It is in the form of distinctly invasive carcinoma.
The terms cervical intraepithelial neoplasia (CIN) or squamous intraepithelial lesion (SIL) are used for these precancerous changes. In most women, these precancerous changes disappear or remain unchanged, however, when treated, almost all cervical cancers will be prevented.
Cervical cancer occurs between the ages of 35-55 on average, but since there is a risk of developing cancer over the age of 65, all sexually active women or women over the age of 18 should be screened regularly until at least 70 years of age. A sexually transmitted virus called Human Papilloma Virus (HPV) has been detected in almost all cervical cancer lesions. For this reason, it is thought that vaccines developed against this virus will be effective in preventing cervical cancer.
Major Risk Factors for Cervical Cancer:
Infection of the cervix with high-risk Human Papilloma Virus (HPV): It is reported that 3 out of 4 people between the ages of 15-49 have HPV infection at some point in their lives. The infection may not show symptoms for years, it may not always cause genital warts, but this does not mean that the person does not carry the virus. Infection may not always progress to cancer, but high-risk oncogenic HPV types cause changes that can cause cancer later. For this reason, frequent follow-up is recommended for people with HPV detected.
Having sexual intercourse at an early age (before the age of 20), having multiple sexual partners or having intercourse with a person with multiple sexual partners: People who are HPV carriers are usually unaware of their condition, as cancer often does not show symptoms before it develops. For this reason, the only and sure way to prevent HPV is to be monogamous or not to have intercourse with people who are likely to be HPV carriers. Condoms do not protect against HPV.
Smoking: The risk is doubled compared to non-smokers.
Other risk factors: diseases that weaken the immune system, chlamydia infection, low socioeconomic level, not having regular pap smear tests..
What are the Symptoms of Cervical Cancer?
Precancerous lesions are usually asymptomatic, but symptoms occur when the cells turn into cancer and spread to the deep parts of the cervix and adjacent organs. In the early stages of cervical cancer, bloody and foul-smelling vaginal discharge, pain during sexual intercourse or vaginal bleeding afterwards, excessive and prolonged menstrual bleeding can be seen. These findings may also be due to reasons other than cervical cancer, but they should not be neglected and a doctor should be consulted to avoid delay in treatment.
How is Cervical Cancer Diagnosed?
Pelvic Examination: In the gynecological examination, the doctor evaluates the vagina, cervix, uterus, ovaries, fallopian tubes and bladder in order to detect pathological changes. The best way to detect cervical cancer at an early stage is to have a regular pap smear test. Pap smear test is the process of taking cells as a swab from the endocervical canal with the help of a brush during the gynecological examination and the pathologist evaluates whether these cells are suspicious under the microscope. If the doctor detects abnormal changes in the cervix during the pelvic exam and Pap smear test, they may repeat the Pap smear test. If the test is positive, that is, if it contains abnormal cells, the doctor may recommend HPV DNA test, colposcopy. Some HPV types, such as HPV16 and HPV18, are more common in women with cervical cancer and can help confirm the diagnosis. However, many women carry HPV, so HPV testing alone is not a definitive enough test for cervical cancer. However, if Pap smear tests show some cellular abnormalities and the HPV test is positive, the doctor may recommend additional diagnostic tests (colposcopy).

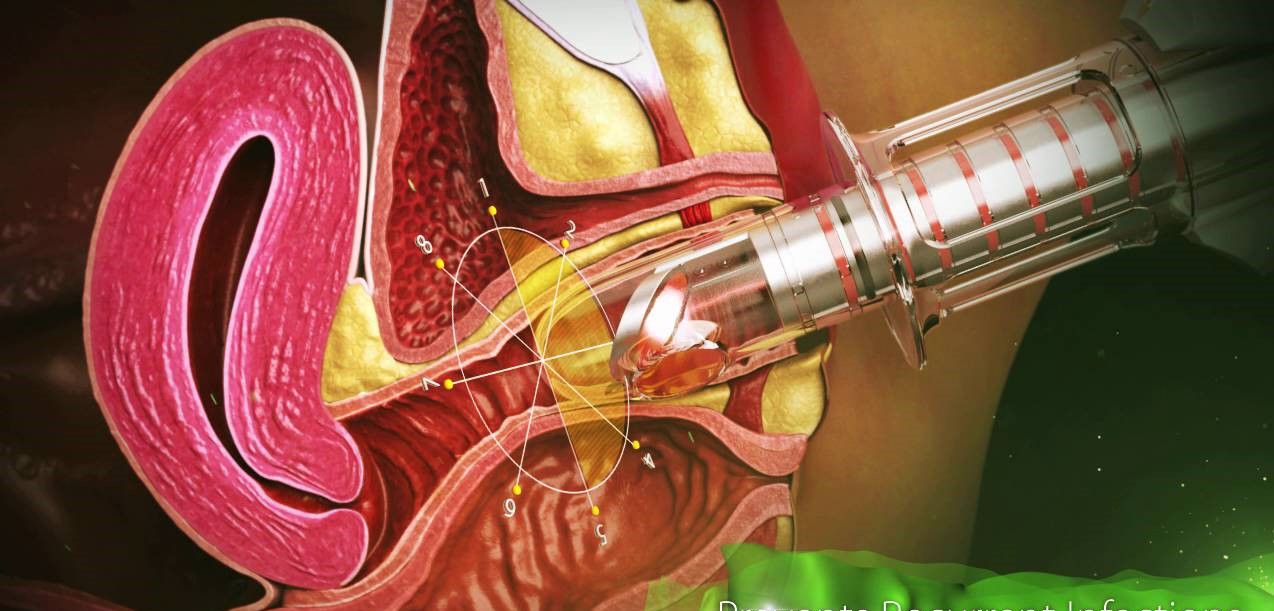
Since the Pap smear test is a screening test, further tests such as colposcopy, biopsy, and endocervical curettage (ECC) will be required for definitive diagnosis in the presence of an abnormal result. Colposcopy is a method of examining the cervix in more detail by a special lighted magnifying glass. During colposcopic examination, a biopsy can be taken from suspicious areas by applying 5% acetic acid and lugol solutions to the cervix surface, and biopsies are evaluated by the pathologist.
Suspicious areas detected by colposcopy are removed with techniques such as cryotherapy (freezing), LEEP or laser. These treatments are always effective in destroying precancerous lesions and preventing cancer. However, regular pap smear screening should be continued to monitor for recurrence of abnormal changes.
Cervical Cancer Treatment:
Mild dysplasia (CIN I): Colposcopy (+/- biopsy) is performed. It is recommended to have a Pap smear every 4-6 months. Most cases regress spontaneously. If mild dysplasia (CIN I) does not regress in the follow-ups, it is recommended to repeat the colposcopy, take a biopsy, and perform cryotherapy or laser vaporization.
Moderate dysplasia (CIN II) and Severe Dysplasia (CIN III): Colposcopic biopsy and endocervical curettage are performed. If invasive cancer is ruled out as a result of the pathological examination of the biopsies, local conservative treatment is performed with cryotherapy, CO2 laser and LEEP conization. Total removal of the uterus (hysterectomy) is recommended in women who have completed their fertility.
When precancerous cell changes are detected in the cervix, the pathology is limited to the cervical epithelium. There is no possibility of spread (metastasis). In cervical cancer, cancer cells fill the entire epithelial layer and progress to the subepithelial layer. There is a possibility of distant organ metastasis via lymphatic pathways.
Histopathological type of cervical cancers are 80-85% squamous cell cancers. 15-20% of adenocarcinomas are seen. Other histological types are rare.
5-year survival rate in cervical cancer is 72%. The course and treatment of cervical cancer are determined by factors such as the histopathological type and degree of the cancer, the stage of the disease, the age of the patient, the general condition, and the rate at which the disease spreads. For this purpose, tests such as blood count, chest X-ray, intravenous pyelography, cystoscopy and rectoscopy are performed.
Usually Radical surgical treatment, Radiotherapy or a combination of these are performed. In some cases, chemotherapy may be added to the treatment.
Radical Hysterectomy: It is the standard treatment for stage 1a2,1b and IIa cases. Radical hysterectomy and pelvic-paraaortic lymphadenectomy, called Wertheim-Meigs operation, are performed. In young women, the ovaries can be preserved because less than 1% of cervical cancers metastasize to the ovary.
Radiotherapy: Radiation therapy is the use of high-energy x-rays or other particles to kill cancer cells. RT has a place in every stage of cervical cancer. Radiotherapy can be applied before or postoperatively to shrink the tumor. An external or intracavitary high-energy beam is sent to the area of the tumor. A combination of radiotherapy and chemotherapy can also be done.
Chemotherapy is a systemic drug therapy used to kill cancer cells that have spread to other parts of the body. Chemotherapy travels through the bloodstream in the body towards tumor cells. The goal of chemotherapy may be to slow the growth of the tumor, destroy any remaining cancer after surgery, or reduce tumor-related side effects.
Although chemotherapy can be given orally (by mouth), most drugs used to treat cervical cancer are given intravenously (by IV). IV chemotherapy is injected directly into a vein or through a catheter. Because chemotherapy affects normal cells as well as cancer cells, many people experience side effects from the treatment.
The side effects of the treatment in cervical cancer vary depending on the type of surgical operation, whether or not he received radiotherapy, the drugs used in chemotherapy and the duration of the treatment.
After Cervical Cancer Treatment:
The recurrence probability of the tumor in the first 2 years after cervical cancer treatment is 74%. For this reason, patients should be checked with gynecological examination and smear every 2-4 months after treatment. At the end of the 1st year, chest X-ray and Computed Tomography are taken.
What are the Ways of Protection from Cervical Cancer?
Most precancerous lesions and cervical cancers can be prevented with regular Pap smears. Preventing precancerous lesions means controlling risk factors:
Delaying the age of first sexual intercourse
Limiting the number of sexual partners
Avoiding sexual intercourse with people with a large number of partners
avoiding sex with people who have genital warts or show signs of other sexually transmitted infections
Having safe sex using a condom will both reduce the risk of HPV infection and protect against HIV and AIDS.
quit smoking
Have a regular pap smear test (The Pap test is the most common test to screen for cervical cancer.)
Is Cervical Cancer Contagious?
Cervical Cancer itself is not contagious. However, the cancer-causing HPV virus (Human Papillomavirus) is highly contagious. HPV virus is quite common in both men and women and they are carriers. Condoms should always be used to prevent HPV transmission, but since HPV is transmitted by skin-to-skin contact, condom use does not protect you 100%. HPV Vaccines are commercially approved for the prevention of certain types of viruses that are responsible for cervical cancer.
False Information and Truths About Cervical Cancer (Cervical Cancer)
Cervical cancer (cervical cancer) is a type of cancer that we are not comfortable talking about openly, that can be misinformed by hearsay and that can be affected emotionally.
FALSE 1: Cervical Cancer is Unpreventable
TRUE: Cervical Cancer is one of the most preventable cancers. There is a vaccine against the most common strains of HPV (HPV Type 6-11-16-18) to reduce the chance of virus transmission. However, those who have been vaccinated should also have regular pap smear tests to be screened for other strains of HPV.
FALSE 2: Cervical Cancer Is Hereditary
TRUE: Unlike breast cancer, cervical cancer is not hereditary. Even if no family members have the disease, this does not mean that you are not at risk.
FALSE 3: I’m Too Young to Have Cervical Cancer.
TRUE: Even if you’re in your 20s, you can get cervical cancer.
FALSE 4: I am not a sex addict
. TRUE: Even if you are monogamous, you can get cervical cancer.
FALSE 5: When I have cervical cancer, my uterus needs to be removed, so I cannot have children after treatment.
TRUE: Treatment depends on the stage of the cancer. If the cancer is detected at an early stage, only the cancerous areas will be removed with minor surgery, it will not affect your ability to have a baby in the future. However, if the cancer is detected at an advanced stage or has spread widely, radiotherapy or hysterectomy (removal of the uterus) may be necessary. Only this group of patients will not be able to get pregnant. For this reason, it is extremely important to detect cervical cancer at an early stage.
Appointment and Contact Information for Jin.Op.Dr.Yeşim Yerçok (Gynecology and Obstetrics Specialist) :
Phone: +90 216 385 17 15
Address: Fener Kalamış cad. Billur apt. No:5 Da:9 Kiziltoprak – Kadıköy / İSTANBUL
E-Mail:
info@dryesimyercok.com