An ectopic pregnancy is the implantation and growth of the fertilized egg outside the uterus, not inside the uterus. Ectopic pregnancy was first described in the 11th century and although a fatal condition until the advent of surgery and blood transfusions in the early 20th century, advanced diagnostic tools and surgical methods have been developed since the 1970s with modern drug treatments. Thus, not only the woman’s life is preserved, but also her future reproductive ability.
How Does an Ectopic Pregnancy Occur?
In each woman, 1 egg is produced each month and goes on a journey to meet the male sperm in the fallopian tube and become fertile (fertilization). In a normal pregnancy, the fertilized egg (zygote) completes its journey in the fallopian tube and reaches the uterus within 3-5 days. The zygote continues to grow, attaching securely to the uterine wall (implantation). In the first 2 months of its development, it transforms from zygote to embryo.
In an ectopic pregnancy, the fertilized egg cannot make this journey because there is a narrowing or blockage in the fallopian tube. The fallopian tube is not large enough for the zygote to grow. Eventually, the thin walls of the tube are stretched and burst (rupture). The result is severe bleeding and perhaps death. More than 95% of all ectopic pregnancies occur in the fallopian tube. It is seen in the abdominal (abdominal cavity) only 1.5%, less than 1% in the ovary (ovary) or cervix (cervix). According to the region where the ectopic pregnancy is located, it is defined as tubal pregnancy, ovarian pregnancy, cervical pregnancy and abdominal pregnancy.
Ectopic pregnancy, also known as ectopic pregnancy, is seen in 1 out of 60 pregnancies.
Ectopic pregnancies often occur when there is a problem with the journey of the fertilized egg from the fallopian tube to the uterus. Ectopic pregnancy is more common in women aged 35-44.
What are the Causes of Ectopic Pregnancy?
50% of women who have had an ectopic pregnancy have a history of pelvic inflammatory disease (PID). This is an infection of the fallopian tubes (salpingitis), which can spread to the uterus and ovaries. It is usually caused by Gonorrhea and Clamydia infections, and these are usually transmitted through sexual intercourse. Infections cause damage or blockage in the fallopian tube. Normally, the inside of the fallopian tube is lined with tiny hair cells called cilia. These cilia are important in the easy progression of the egg from the ovary to the fallopian tube and then into the uterus. If the cilia are damaged by infection, the transfer of the egg is interrupted. The fertilized egg implants in the fallopian tube before it reaches the uterus, resulting in an ectopic pregnancy.
Other Conditions Increasing the Risk of Ectopic Pregnancy:
- endometriosis. It is when normal intrauterine tissue is found outside of the uterus, which can block the fallopian tubes.
- Fetal exposure to Diethylsilbestrol (DES). If the woman took DES (the synthetic version of the estrogen hormone) during her pregnancy, the baby girl in her womb may have an anomaly in her tubes, and when this girl becomes pregnant in the future, she may experience an ectopic pregnancy due to an abnormality in her tubes.
- Taking hormones: Estrogen and progesterone hormones can be used for contraception or other reasons as well as regulating the menstrual cycle. These hormones also affect the fallopian tube and can cause the fertilized egg to move slowly in the fallopian tube. Even women who use progesterone-only contraceptives have a higher risk of ectopic pregnancy. Ectopic pregnancy can also be seen in the intake of ovarian stimulating hormone for IVF.
- Using an intrauterine device (Spiral): This contraceptive method was developed to prevent implantation of the fertilized egg into the uterus. However, it does not prevent the development of ectopic pregnancy. In addition, if the woman becomes pregnant while using an IUD for contraception, the fertilized egg will be implanted elsewhere in the uterus (50%). However, the relationship between IUD and ectopic pregnancy is weak, since the probability of getting pregnant with an IUD is extremely low.
- Surgery of the fallopian tube: The risk of ectopic pregnancy is high (60%) in women who become pregnant after tubes are tied to prevent pregnancy. In addition, surgical interventions for reopening the tubes after ligation increase the risk of ectopic pregnancy.
- History of previous ectopic pregnancy (probability increases by 15% after the first ectopic pregnancy and 30% after the second ectopic pregnancy)
- Repeated abortion history
- Smoking increases the risk of ectopic pregnancy. This risk is dose dependent, the number of cigarettes smoked increases the risk.
What are the Symptoms of Ectopic Pregnancy?
- Stomach ache
- Menstrual delay or absence of menstruation
- Vaginal bleeding or intermittent spotting
The woman may not be aware that she is pregnant. Symptoms are typical in ruptured ectopic pregnancy (with severe internal bleeding) and non-ruptured ectopic pregnancy (not yet burst). However, these symptoms may also occur in other situations (abort-miscarriage).
Signs and symptoms of ectopic pregnancy appear 6-8 weeks after the last menstrual period. If the ectopic pregnancy is not in the fallopian tube, these symptoms may appear later. Other pregnancy symptoms (eg nausea, breast tenderness, etc.) may also be seen in ectopic pregnancy. Fatigue, dizziness and fainting may indicate severe internal bleeding and low blood pressure in a ruptured ectopic pregnancy and require immediate medical treatment. Unfortunately, the symptoms in a bleeding ectopic pregnancy may go unrecognized and this may cause the patient to go into shock (low blood pressure, weak and rapid pulse rhythm, pale skin and unconsciousness) and require immediate treatment.
Pain in an ectopic pregnancy is often the first symptom. Pain is often unilateral, felt in the pelvis, in the abdominal cavity, and even shoulder or neck pain may be present. (Blood leaking from a ruptured ectopic pregnancy accumulates under the diaphragm and the pain can be described as shoulder and neck pain) The pain is usually sharp and stabbing. The biggest concern in an ectopic pregnancy is internal bleeding into the abdominal cavity. In any doubtful case, an emergency treatment plan should be initiated. Weakness and dizziness may indicate serious internal bleeding that requires immediate medical attention.
Early Symptoms
All hormonal changes in an ectopic pregnancy are the same as in a normal pregnancy; Fatigue, nausea, delayed menstruation, breast tenderness, low back pain, mild cramping pain on one side of the pelvis and abnormal vaginal bleeding, often spotting.
Late Symptoms
When the embryo grows too large within the narrow space of the fallopian tube, the first sign that something is wrong is stabbing pain in the pelvis or abdomen. If the tube ruptures (bursts), the blood irritates the diaphragm and causes shoulder pain. Other warning signs are dizziness and fainting.
Is there a menstrual period in an ectopic pregnancy?
Often the first warning sign of an ectopic pregnancy is vaginal bleeding and pain. The pain may be felt on only one or all sides of the abdomen, shoulder, neck, or pelvis, and may be mild or sharp in intensity.
In an ectopic pregnancy, the vaginal spotting seen after menstrual delay may be mistaken for menstrual bleeding, but the accompanying dizziness, fainting and low blood pressure are due to blood loss. Severe back pain is experienced.
How Is Ectopic Pregnancy Diagnosed?
The first step in diagnosis is examination and evaluation by the doctor. Step 2 is the pregnancy test.
In the early period of ectopic pregnancy, the doctor determines that the patient is pregnant, but the embryo is not in the uterus. The doctor may detect a mass and pain in the abdomen during the pelvic evaluation.
Some blood tests are helpful in making a diagnosis. Measurement of Human chorionic gonadotropin (hCG) level in the blood is the most useful test in the early stages. In a normal pregnancy, in the first 10 weeks of pregnancy, the hCG level increases 2 times every 2 days. In ectopic pregnancy, however, the hCG level rise is much slower and the level is lower than normal. (This finding can also be seen in pregnancies that ended in miscarriage). Progesterone levels in the blood can also be measured. Levels lower than expected may detect that the pregnancy is not normal.
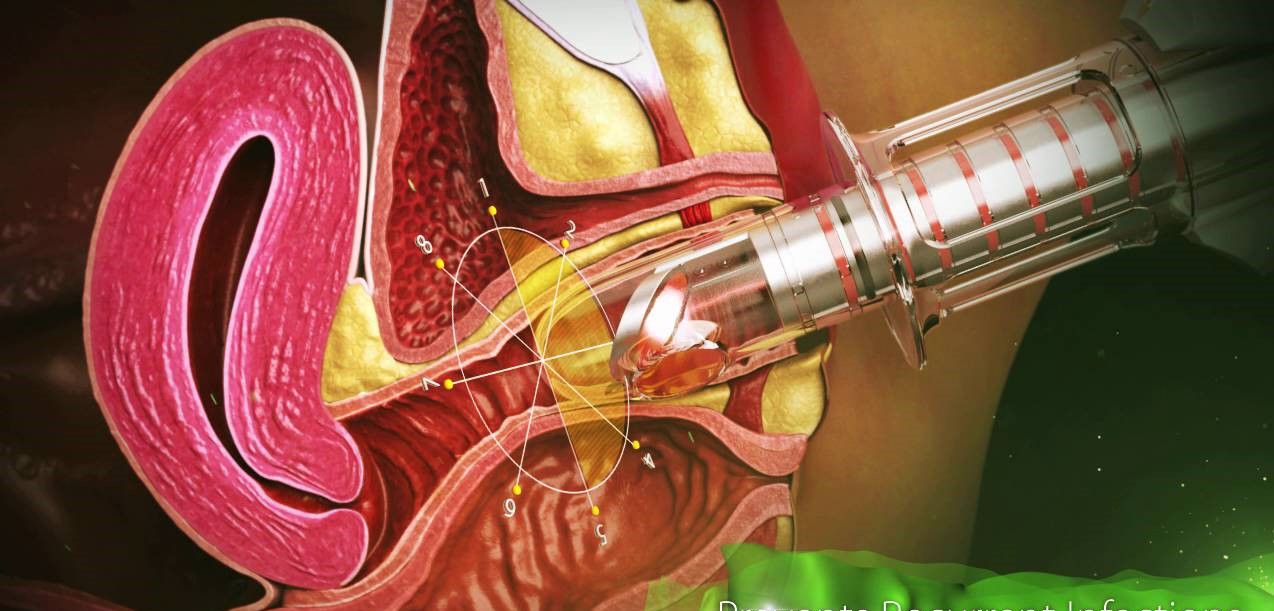
Ultrasound evaluation provides information about whether the pregnancy is an ectopic pregnancy. An image is formed on the screen when high sound waves placed inside the patient’s vagina by means of a transducer or sent from the abdominal (abdominal) surface are evaluating the internal organs. The doctor needs to see if a fetus is developing in the womb at least 3-5 weeks after fertilization.
Culdocentesis also helps in making the diagnosis. In this procedure, the needle inserted from the posterior apex of the vagina evaluates the back of the uterus and the area in front of the rectum. This area is where blood from the ruptured fallopian tube accumulates. Seeing blood coming from this area through the needle helps us to diagnose.
Through laparoscopy, the doctor can evaluate the reproductive organs of the patient in the pelvis and detect an ectopic pregnancy. In this technique, a thin tube with a light and camera at the end is sent into the abdomen through a small incision made in the abdomen. This instrument helps to see and evaluate the organs in the abdomen.
How Is Ectopic Pregnancy Treated?
An ectopic pregnancy requires immediate treatment. Early treatment is the best chance to preserve the tube for future pregnancies.
Medication
If an ectopic pregnancy is discovered at a very early stage, a drug called Methotrexate may be given. For best results, pregnancy should be less than 6 weeks and tubal mass diameter should not exceed 3.5 cm. Beta-subunit (HCG) level should be less than 5000 mIU/mL in methotrexate treatment. It is 90% effective in the treatment of ectopic pregnancy.
Methotrexate therapy has been used successfully since 1987. It works on the principle of inhibiting the growth of rapidly growing zygote cells. It is also used in the treatment of certain cancers). Most side effects are mild and transient, but the patient should be monitored after treatment. Usually, the drug is administered intramuscularly as a single dose. But it can also be given intravenously or directly into the embryonic tissue located in the fallopian tube. Methotrexate can also be used in the treatment of ovarian, abdominal and cervical pregnancy detected in the early stages.
Surgical treatment
When an ectopic pregnancy is detected in laparoscopy, some surgical instruments are inserted into the abdomen through a small incision made on the abdominal skin to remove the ectopic pregnancy mass. The affected fallopian tube can be repaired or removed if necessary. Most patients and doctors prefer the laparoscopy method because the small incision (incision) helps faster recovery. However, in some severe cases, laparoscopy is not sufficient or appropriate. Laparoscopy is not performed in severe adhesions or severe blood loss in the abdomen. Damage to the fallopian tube or localization of pregnancy may require laparotomy.
If the pregnancy has ruptured, laparoscopy or laparotomy (a transverse incision from the area we call the bikini line) is performed, and it is urgently planned to stop the blood loss and remove the embryo. Every effort is made to preserve and repair the affected fallopian tube. However, if the fallopian tube has ruptured, it is extremely difficult to repair, so removal is usually preferred.
After an Ectopic Pregnancy?
Ectopic pregnancies constitute 9% of all pregnancy-related deaths in the United States and cause death in the first trimester (first 3 months). More than 1% of ectopic pregnancies can result in death. If an ectopic pregnancy is detected and treated early, the outcome is very good.
Can an Individual Who Had an Ectopic Pregnancy Conceive Again?
The chances of a healthy pregnancy are low after an ectopic pregnancy, but this depends on the degree of permanent damage to the fallopian tube. If the tube is left, the chance is more than 60%. If one of the tubes is removed, the egg will be fertilized in the other tube, the chance of a successful pregnancy is 40%.
How to Prevent Ectopic Pregnancy?
There are many forms of ectopic pregnancy and it cannot be prevented. However, tubal pregnancies, which account for the vast majority of ectopic pregnancies, can be prevented by avoiding conditions that cause damage to the fallopian tubes. Since half of all women who have had an ectopic pregnancy have a history of PID, protection from sexually transmitted diseases, early diagnosis and treatment reduce this risk.
Although very rare, an ectopic pregnancy can occur at the same time as an ectopic pregnancy. We call this condition “heterotopic pregnancy”. The frequency of heterotopic pregnancy has increased in recent years due to IVF (in vitro fertilization) and other assisted reproductive techniques (ART).
Molar pregnancy is different from ectopic pregnancy. A molar pregnancy is the growth of a grape-shaped mass in the uterus, which usually develops from an egg encoded with abnormal genetic information.
Jin.Dr.Yeşim Yercok
Gynecology Obstetrics and IVF Specialist
For appointment Tel: 0216-3851715
Address: Fener Kalamış Cad. Billur apt. No:5 Da:9 Kiziltoprak/ Istanbul