Genital Herpes
İçindekiler
- 1 What is Genital Herpes?
- 2 What Causes Genital Herpes?
- 3 What Are the Symptoms of Genital Herpes?
- 4 How Is Herpes Diagnosed?
- 5 How Is Genital Herpes Treated?
- 6 How Common Is Genital Herpes?
- 7 Can Herpes Be Completely Eliminated?
- 8 HIV and Genital Herpes
- 9 Possible Complications
- 10 When Should I Apply for a Doctorate?
- 11 How to Catch Genital Herpes?
- 12 How Can I Avoid Genital Herpes?
- 13 How to Prevent Transmission of Genital Herpes to Others?
- 14 How Does Genital Herpes Affect Pregnant Women and Their Baby?
What is Genital Herpes?
Genital herpes caused by HSV (Herpes Simplex Virus); It is a viral disease that is spread by the contact of the mucous membranes in the mouth, vagina or genital area and falls into the class of sexually transmitted diseases. Genital herpes is an infection that affects the genitals (penis in men, vulva and vagina in women) and the surrounding area (buttocks and anus).
What Causes Genital Herpes?
Two types of Herpes Simplex Virus cause genital lesions: HSV-1 and HSV-2.
HSV-1 often causes blisters in the mouth area, while HSV-2 causes genital sores or lesions around the anus. The emergence of herpes is closely related to the immune system. In women with weakened immune systems (due to stress, infection or drugs), the disease is more frequent and prolonged.
- Herpes simplex virus type-1 (HSV-1) This virus is mostly seen as an infection on the lips, mouth and face. It is the most common form of herpes simplex and many people get it from childhood. HSV-1 often causes sores, blisters, or infections of the eyes (especially the conjunctiva and cornea) in the mouth. It can also lead to infection of the brain (meningoencephalitis). It is transmitted by contact with infected saliva, saliva. In adult life, 30-90% of people develop antibodies. It is more common in societies with low socioeconomic status.
- Herpes simplex virus type-2 (HSV-2) This virus is usually transmitted through sexual intercourse. Symptoms are in the form of ulcers and sores in the genital area. However, some people with HSV-2 may not have symptoms. It can cause Type 1 and Type 2 cross-infection with mouth-genital area contact. In other words, you can get genital herpes from your mouth and oral herpes from your genital area.
Genital herpes is only spread from person to person by direct contact. 60% of sexually active adults are believed to have the disease
What Are the Symptoms of Genital Herpes?
Herpes symptoms are similar in men and women. When exposed to the virus, there is an incubation period, usually 3-7 days, before the lesion develops. During this time, there are no symptoms and the virus is not transmitted to other people. Usually, the first infection occurs within 2 weeks, and the symptoms appear as itching and tingling sensations, followed by redness of the skin. Eventually, a bubble (vesicle) appears. When the blisters burst, they turn into ulcers that are very painful to touch, usually within 7-15 days. The infection is absolutely contagious from the day the itching starts until the ulcer heals completely, usually lasting 2-4 weeks. However, infected individuals can transmit the virus to their sexual partners even when there are no apparent signs of illness.
In most patients, inflammation of the cervix (cervicitis) may occur, and in some women, cervicitis may be the only manifestation of herpes.
Some women with genital herpes may complain of painful urination, which may be the cause of inflammation of the urethra (urethritis).
Symptoms vary depending on whether the infection is ‘first time’ or ‘recurring’. For the first time, symptoms of primary infection are usually worse. However, new HSV infection may be asymptomatic in most cases. Studies have shown that 10-25% of people infected with HSV-2 are unaware of the presence of genital herpes. Even infected people with mild or no symptoms can become infected with the herpes virus.
Primary Genital Herpes: The first symptoms are usually seen in or around the genital area 1-2 weeks after sexual intercourse. There is a tingling or stinging sensation in the affected areas (genital, buttocks or inside the legs), blisters appear in groups at the site of small rashes. After 2-3 weeks, the blisters multiply and burst into painful open sores. The lesions dry out after a while, crust over and heal quickly without leaving any traces. Blisters in moist areas will heal more slowly. Lesions may itch, but scratching reduces healing.
40% of men and 70% of women may experience other symptoms of genital herpes (flu-like discomfort, headache, muscle pain, fever, and swollen glands in the groin-neck). Some patients have difficulty urinating and vaginal discharge in their name.
Recurrent Genital Herpes: Generally, recurrent lesions are milder and of much shorter duration (3 weeks for primary infection, 3 days for recurrent infection). There may be only mild itching in women, while it is much milder in men. On average, a person experiences 4 relapses in 1 year. Over time, the frequency of recurrence decreases.
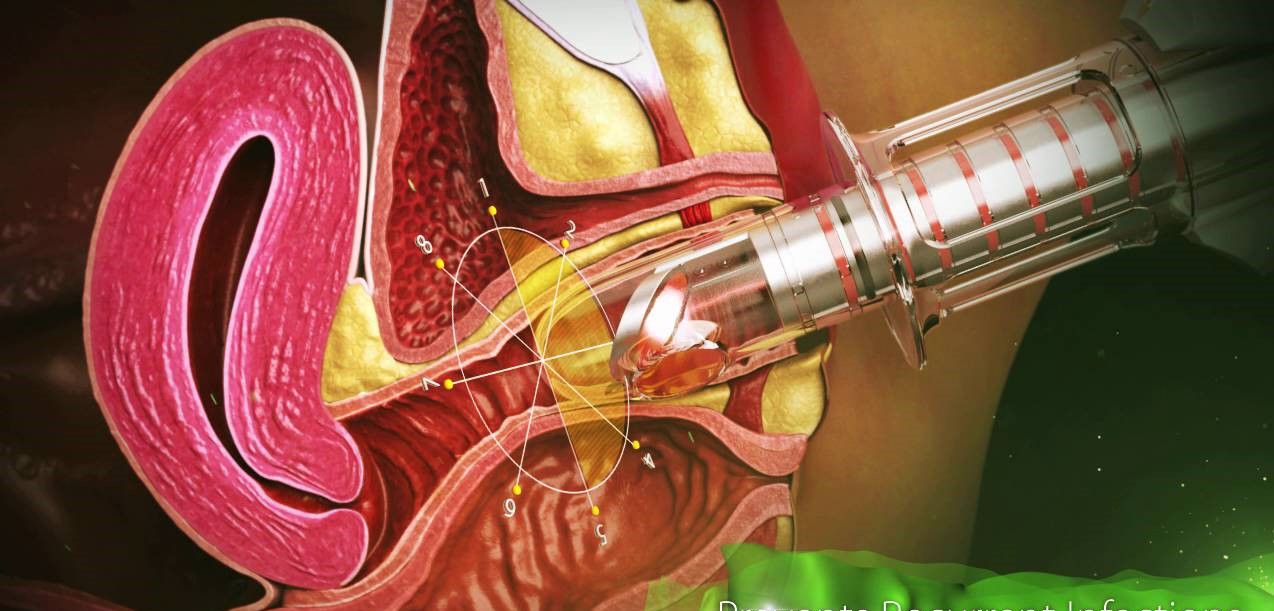
How Is Herpes Diagnosed?
Herpes simplex virus is usually recognized by its characteristic lesions: thin-walled, water-filled blisters on reddened skin. However, many other diseases can resemble herpes, and a doctor may not rely solely on visual assessment to diagnose herpes. Also, some patients with the virus may have no visible lesions. Laboratory tests are required to confirm the diagnosis of herpes. These tests are:
Virological tests (viral culture from the lesion)
Serological tests (blood test for antibody detection)
The Centers for Disease Control (CDC) recommends both tests for the diagnosis of genital herpes. However, other sexually transmitted diseases should also be screened in patients diagnosed with genital herpes.
At the first signs of disease, a sample of fluid from the blisters can be sent to the laboratory for culture. However, the culture is positive in only 50% of infected patients. On the other hand, a negative result does not mean that it is not a virus. However, a positive response is highly reliable when a sample is taken from the fluid-filled blister at an early stage, before it has dried or crusted over.
Virological Tests
Viral tests are done by taking a fluid sample or culture from the lesion. It is done in the early period, ideally within the first 3 days after it becomes visible. If there is a virus, it will grow in this liquid in 1-10 days. If the infection is severe, this reproduction occurs within 24 hours. The viral culture test gives a very accurate response if the lesions are in the stage of a clear, fluid-filled blister (vesicle), but the test will not work properly if the lesions are old ulcerated sores or recurrent lesions.
Polymerase chain reaction (PCR) tests are much more accurate than viral cultures, and the CDC recommends using this test to look for herpes in the spinal fluid in the diagnosis of herpes encephalitis. PCR can make a diagnosis by copying the virus DNA even if a very small amount of DNA is present in the sample. PCR is much more expensive than viral culture and the FDA has not approved it for use in genital specimens. However, because PCR is extremely sensitive, many laboratories use this test to diagnose herpes.
Tzanck smear test is an old-style virological test, it is used by scraping from the herpes lesion, examined under a microscope. Multinucleated giant cells or virus-carrying particles (inclusion body) are specific findings. It is a quick test but only 50-70% accurate. This test cannot distinguish between Herpes simplex or Herpes Zoster. The Tzanck test is not reliable in the definitive diagnosis of herpes infection and is not recommended by the CDC.
Serological Tests
Serologic (blood) tests identify antibodies specific to the virus and its type (HSV-1 and HSV-2). When the herpes virus infects someone, the immune system (immune system) in that person’s body produces special antibodies to fight the infection. If the blood test has detected antibodies to Herpes, it is proof that you are infected with this virus, even if the virus is in the latent (non-active) stage. This means you carry the virus and can infect others.
There are 2 different proteins associated with the herpes virus.
- Glycoprotein gG-1 (HSV-1)
- Glycoprotein gG-2 (HSV-2)
Glycoprotein (gG) type-specific tests have been used since 199. The CDC recommends type-specific glycoprotein (gG) tests for the diagnosis of herpes.
Serological tests are most accurate when performed 12-16 weeks after exposure to the virus.
Recommended Tests:
HerpeSelect: Includes two tests: ELISA (enzyme-linked immunosorbent assay) or Immunoblot test. These two tests give very accurate results in the detection of both types of Herpes Simplex Virus. However, since the samples have to be sent to the laboratory, the office type Biokit results in longer time than the tests.
Biokit HSV-2 ( SureVue HSV-2): This test detects only HSV-2. Its main advantage is that it only requires fingertip puncture and the result is achieved in less than 10 minutes. It is an extremely accurate and inexpensive test.
Western Blot Test: It is the gold standard for researchers as its accuracy is 99%. However, it is expensive and time consuming, so its use is not common compared to other tests.
When the tests are done in the early stage of the infection, the results may be wrong, your doctor may recommend repeating the test.
Your doctor may specifically request serological tests to be performed in the following situations:
- Herpes viral culture tests are negative but in people with recurrent lesions
- To confirm the disease in people with visible signs of genital herpes
- If your partner has visible genital herpes or has been diagnosed with genital herpes
- When there is a need for investigation for multiple partners or sexually transmitted diseases
How Is Genital Herpes Treated?
Treatment of genital herpes depends on whether the infection is experienced for the first time (primary infection) or if symptoms of previous infection reappear (recurrent infection).
Antiviral drugs containing aciclovir, famciclovir and valaciclovir can be used in the treatment of genital herpes. These are available in the market under different names. But these drugs cannot completely eliminate the virus from your body. If antiviral therapy is started at the early stage of symptoms, it reduces the severity and duration of symptoms. Acyclovir is the oldest antiviral drug and must be taken 5 times a day. Famciclovir and valaciclovir are newer antiviral drugs and are taken 3 times a day.
HSV recurs in 2/3 of people with Genital Herpes and in 1/3 it recurs 3 or more times per year. HSV can never be completely eliminated from the body, but it can sleep for a while, then become active again and cause symptoms.
Primary Infection
If this is your first time experiencing genital herpes, see your gynecologist. He may need to prescribe some antiviral tablets (such as acyclovir) to be used 5 times a day.
Acyclovir works by preventing HSV from multiplying. However, this medicine cannot completely clear HSV from your body and will not work if you stop taking your medicine.
If you still have new blisters and open sores in your genital area despite starting treatment, you will need to take acyclovir for at least 5 days or more.
Acyclovir may cause some side effects such as headache or feeling unwell.
It can be used to treat genital herpes in other antiviral therapies (famciclovir and valaciclovir)
Recurrent Infection (Recurrent Infection)
If you have had herpes before and think it has recurred, you should contact your doctor. If symptoms are mild, your doctor may recommend things to do at home to relieve symptoms without needing any treatment.
- Keep the affected area clean using water or salt water. Helps prevent blisters or open wounds from becoming infected and heal faster.
- Applying ice cubes or wet, cold tea packs wrapped in a clean cloth to wounds can soothe the pain and help it heal quickly. Do not apply ice directly to the skin.
- Applying Vaseline or anesthetic creams on blisters or sores will reduce your pain when urinating.
- Drink plenty of water to dilute your urine so you will have less painful urination. Urinating while holding water to your genital area or showering also helps.
- Avoid wearing tight clothing to avoid injuring blisters and sores.
If symptoms are severe, an antiviral drug (acyclovir) to be taken 5 times a day should be prescribed.
Topical treatments (applied directly on the lesion) are generally less effective and not routinely used. Medications are taken by mouth or, in severe cases, given iv. It is not possible to completely eliminate genital herpes, it should be remembered that these treatments will only reduce the severity and duration of the disease.
Episodic Treatment
If genital herpes recurs less than 6 times a year, your doctor will give you a 5-day course of acyclovir every time you feel tingling and numbness before symptoms start.
Suppressive Therapy (Suppressive Therapy)
If your genital herpes recurs more than 6 times in 1 year, or if your symptoms are particularly severe and distressing, you may need to take acyclovir daily as part of a long-term treatment plan. This is known as suppressive therapy. In this case, you may need to take it 2 times a day for 6-12 months.
While taking suppressive therapy, the chances of passing on HSV to your partner are reduced, but it is important to remember that it does not prevent it completely.
Suppressive therapy is usually stopped after 12 months. As long as you have occasional mild lesions or when you need it, only a 5-day course of acyclovir is taken. Recurrent genital herpes usually becomes less frequent and mild after 2 years. If recurrent lesions are severe, suppressive therapy is restarted.
How Common Is Genital Herpes?
The CDC estimates that 776,000 people in the United States get new herpes infections each year. Genital herpes is very common in the USA, with 16% nationwide having genital HSV-2 in people aged 14-49 years.
Can Herpes Be Completely Eliminated?
There is no treatment that completely eliminates herpes. Antiviral treatments shorten the duration of the illness while the person is taking the drugs. Also, daily suppressive treatments reduce the transmission of herpes to your partner.
HIV and Genital Herpes
If you have recurrent genital herpes, you should also be investigated for HIV. Because this situation may be a sign of weakening of the immune system (the body’s natural resistance to infections and diseases), it may be a sign of the presence of HIV. Genital herpes is very severe in people with HIV.
Differential diagnosis:
Aphthous Ulcers: The wounds we call aphthous ulcers are often confused with herpes caused by HSV Type-1. Aphthae often occur singly or in groups in the mouth and/or under the tongue. The cause is unknown and may occur in healthy individuals. They are usually white or grayish, crater-like lesions with a sharp border around them with red margins. It heals within 2 weeks without treatment. Aphthous ulcers are quite common.
Candida (Fungus): Candida can cause a whitish infection that grows inside the mouth. Although it is usually seen in infants, it can occur at any age. It is especially common in people who use antibiotics or have a weakened immune system.
Genital diseases: Bacterial infections, genital warts, candida, herpes zoster (shingles), molluscum (a viral disease characterized by small round bumps), scabies, syphilis and some cancers can be confused with genital herpes.
Prognosis: Oral or genital lesions usually heal within 7-10 days. In people with weakened immune systems, the infection can be very severe or long-lasting.
Once an infection occurs, the virus spreads to nerve cells and remains in the body for the rest of a person’s life. It occasionally comes back as symptoms or flare-ups. Relapses can be triggered by excessive sunlight, fever, stress, acute illnesses, drug treatments, and conditions that weaken the immune system (cancer, HIV/AIDS or cortisone use).
Possible Complications
- Herpetic Eczema (widespread herpes across the skin)
- encephalitis
- Eye infection– keratoconjunctivitis
- Infection of the trachea
- Meningitis
- pneumonia
- Prolonged, severe infection in immunocompromised persons
When Should I Apply for a Doctorate?
Call your doctor if your symptoms resemble a herpes infection. There are many different conditions that can cause similar lesions in the genital area.
If you have a history of herpes infection and similar lesions develop again, call your doctor if these lesions do not heal within 7-10 days.
How to Catch Genital Herpes?
It is transmitted when you have sexual intercourse (anal, vaginal or oral sex) with an infected person. HSV-2 can cause sores in the genital area and infections in the mouth and lips. Oral-genital, genital-genital contact with someone who carries HSV-2 in the genital area can cause HSV-2 infection in the genital area.
How Can I Avoid Genital Herpes?
Preventing HSV infection is difficult because people can transmit the virus even if they do not have active visible lesions. Avoiding direct contact with people with visible open lesions will reduce the risk of infection.
People with active genital herpes should avoid sexual intercourse. Using condoms for safe sexual intercourse will reduce the risk of infection. However, the disease can also be seen in areas not covered by the condom.
The surest way to prevent the spread of sexually transmitted diseases such as genital herpes is to avoid sexual contact or to have long-term monogamy with someone you are sure is not infected.
People with active HSV lesions should stay away from newborn babies, children, people with weakened immune systems. Because these people are at high risk and can have the disease much more severely.
To reduce the risk of infection in the newborn, mothers with active HSV infection at the time of delivery may be advised to have a cesarean delivery.
How to Prevent Transmission of Genital Herpes to Others?
- No method can 100% prevent the transmission of the disease to others.
- Do not touch your eyes or mouth after touching blisters or sores.
- In the presence of disease, hands should be washed properly.
- Clothes or linen that come into contact with ulcers should not be shared with others.
- Couples who have an infection in their partner and want to minimize transmission should always use condoms. Unfortunately, it can be transmitted even if the infected partner has no visible lesions.
- Couples may wish to avoid all sexual activity, including kissing, during illness. It is important to avoid sexual contact from the moment the first lesions begin until the lesions are not seen.
How Does Genital Herpes Affect Pregnant Women and Their Baby?
HSV can affect the fetus and cause anomalies. An HSV-infected mother can transmit it to the newborn during vaginal delivery, especially if the mother has active lesions during delivery. However, 60-80% of newborns with HSV infection have no signs of HSV infection in their mothers or a history of genital HSV infection. Transmission of the virus is possible even if there are no symptoms or visible sores.
In pregnant women infected with HSV-1 or HSV-2, sometimes genital herpes infection can cause miscarriage or premature birth (premature birth). Herpes infection can be passed from mother to baby and result in a potentially fatal infection (neonatal herpes). Therefore, it is very important for women to be protected from herpes during pregnancy.
To reduce the risk of disease during childbirth for a woman with genital herpes, the 36th birthday of her pregnancy. Antiviral medication may be recommended during the week. A woman with genital herpes should be carefully examined at the time of delivery, if there are signs of herpes, she should be given a cesarean delivery.
Primary Genital Herpes in Pregnancy:
If the first signs of herpes are seen in the last 6 weeks of your pregnancy or close to the time of delivery, the risk of passing the virus to your baby is very high (25%). Thus, the chance of transmitting the virus to your baby from blisters and sores in your genital area is greatly reduced.
However, if you are determined to have a vaginal delivery instead of a cesarean section, your doctor may start you on antiviral therapy. This drug is given intravenously during labor and delivery.
If you get a primary herpes infection during the first 3 months of your pregnancy (1st trimester), this increases your chances of miscarriage. If you do not get over this period and have a miscarriage, it will not affect your baby’s health.
If the period between contracting the virus and giving birth is more than 2 months, you can have a normal vaginal delivery. Because this is enough time for antibodies to form in your body and it will pass through the placenta to your baby, protecting him from being affected by herpes during birth. Your doctor may prescribe antiviral therapy. These drugs help your wounds heal quickly. Also, some doctors recommend taking antiviral medication during the last 4 weeks of pregnancy to prevent herpes from recurring during delivery. However, this is not routine and the advantages and disadvantages of antiviral therapy should be discussed.
Recurrent (Recurrent) Herpes in Pregnancy
Recurrent episodes of genital herpes do not pose much of a risk to your baby. Even if there are blisters or sores during delivery, your baby’s risk of developing a serious herpes infection is small. Because the antibodies are passed on to your baby.
It is controversial what is best if you have recurrent blisters and sores at the time of birth. Some doctors recommend having a cesarean delivery. However, the National Institute for Health and Clinical Excellence (NICE) argues that cesarean delivery is not necessary in recurrent infection. Likewise, the Royal College of Obstetricians and Gynaecologists (RCOG) do not routinely recommend cesarean delivery, even if there are blisters and sores due to recurrent herpes at the time of delivery. Because the baby has developed immunity to the virus and the chance of developing serious herpes infection is low. If you have a recurrent infection in labor, share your ideas with your doctor and decide together what is the best way to deliver your baby.
The use of antiviral therapy in the last 4 weeks of pregnancy is also controversial. These drugs will prevent the recurrence of vesicles during delivery, but your doctor should weigh the pros and cons.
Most people did not experience any side effects from taking antiviral medication. The most common side effects are nausea, vomiting, diarrhea, abdominal pain and skin rash.
Contact Information with Jin.Op.Dr.Yeşim Yerçok (Gynecologist and Obstetrician) for Genital Herpes Herpes Herpes Treatment :
Address: Fener Kalamış Cad. Billur apt. No:5 Da:9 Kiziltoprak/ ISTANBUL
Phone: +90 216 385 17 15
E-Mail:
info@jinekomed.com