HPV and Genital Warts
İçindekiler
- 1 What is Human Papilloma Virus (HPV)?
- 2 How is HPV Transmitted?
- 3 What are the Symptoms of Human Papilloma Virus (HPV)?
- 4 What is Genital Wart? What are the Symptoms of Genital Warts?
- 5 How to Treat Genital Warts?
- 6 How to Protect from HPV?
- 7 Is There a Diagnostic Test for Genital Warts and HPV?
- 8 Can a Baby Get HPV During Birth?
What is Human Papilloma Virus (HPV)?
HPV is one of the sexually transmitted viruses. It is the most important etiological agent in the development of cervical cancer. Studies have shown that 99% of cervical cancer (cervical cancer) cases are caused by some types of HPV.
How is HPV Transmitted?
Since HPV infection is sexually transmitted, any sexually active woman or man can get HPV infection. It has been reported that 3 out of 4 people between the ages of 15-49 have HPV infection at some point in their life. In order for HPV to be transmitted, it is not necessary to have a full sexual intercourse, even a short-term contact of infected areas with each other is sufficient for transmission. The latent period of this slow-growing virus is 3-12 months, but during this period when no lesions are seen, the disease can be transmitted sexually. In cases where active genital lesions are present, the contagiousness is very high.
What are the Symptoms of Human Papilloma Virus (HPV)?
HPV causes warts in humans. There are more than 50 types of HPV that are transmitted to humans, some of them are sexually transmitted and cause the formation of wart-shaped masses called condyloma acuminatum (condyloma) in the genital area. 15% of sexually transmitted HPV types are carcinogenic.
People with HPV often do not realize they are infected. Infection may not cause symptoms for years, it does not always cause genital warts. Therefore, the absence of warts in the genital area does not mean that the person does not carry the virus. Oncogenic types of HPV that are associated with cancer can cause cervical cancer in women.
HPV is a small, circular, double-stranded DNA virus that belongs to the family papovaviridae. More than 200 of HPV
More than one type has been defined and 40 of them are known to infect the genital tract.
Low oncogenic risk HPV types: 6, 11, 42, 43, 44, 54, 61, 70, 72, 81,
Intermediate risk HPV types: 26,53,66
High-risk HPV types: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, 82.
While low-risk groups cause anogenital condylomas, which we call warts, and low-grade squamous intraepithelial lesions (LGSIL), high-risk groups constitute anogenital cancers and are detected in 99.7% of cervical cancers.
Among oncogenic HPV types, 16 and 18 are responsible for 52% of cervical intraepithelial neoplasia (CIN) and 77% of cervical cancers, while HPV 6 and 11 are responsible for 90% of anogenital condylomas.
The entry of the infection is usually through the skin damaged by friction. Although the use of condoms somewhat reduces the passage, it is not completely protective.
What is Genital Wart? What are the Symptoms of Genital Warts?
HPV (Human Papilloma Virus) causes genital warts. Most genital warts are caused by HPV types 6 and 11, these HPV types are considered “low oncogenic risk,” meaning they have a low potential to cause cancer. Viral particles penetrate the skin and mucosal areas as a result of friction in the genital area during sexual activity. Cells can remain silent for months after being invaded by HPV.
 Genital warts (condyloma) often occur after unprotected sex with a previously infected partner. They can be in a single region with cauliflower appearance in the genital area in both women and men, or they can be widely distributed as a small pinhead. When many warts come together, they are painless tan or gray-colored masses ranging from 1 millimeter to several centimeters (sometimes 15-20 cm in diameter). It is most commonly observed between the active sexual ages of 17-33 years. Genital warts or condylomas are highly contagious. Although genital warts are painless, they can be uncomfortable depending on their location, size and itching. In women, it occurs most often in the labia minora and moist areas of the genital opening, vulva (external genitalia), anus (anus), It is found in the vagina and cervix (cervix) regions. In men, it is seen in the penis, urethra, scrotum, inguinal and rectal region. Warts may appear as soft, raised masses with a smooth (on the penile surface) or protruding (around the anus) surface. Although warts cause visual distress in people, they can also bring along complaints such as pain, bleeding and itching. These lesions should be treated because of the prevention of transmission to the sexual partner and the complaints they cause. 20% of people with genital warts also have other sexually transmitted diseases. Although warts cause visual distress in people, they can also bring along complaints such as pain, bleeding and itching. These lesions should be treated because of the prevention of transmission to the sexual partner and the complaints they cause. 20% of people with genital warts also have other sexually transmitted diseases. Although warts cause visual distress in people, they can also bring along complaints such as pain, bleeding and itching. These lesions should be treated because of the prevention of transmission to the sexual partner and the complaints they cause. 20% of people with genital warts also have other sexually transmitted diseases.
Genital warts (condyloma) often occur after unprotected sex with a previously infected partner. They can be in a single region with cauliflower appearance in the genital area in both women and men, or they can be widely distributed as a small pinhead. When many warts come together, they are painless tan or gray-colored masses ranging from 1 millimeter to several centimeters (sometimes 15-20 cm in diameter). It is most commonly observed between the active sexual ages of 17-33 years. Genital warts or condylomas are highly contagious. Although genital warts are painless, they can be uncomfortable depending on their location, size and itching. In women, it occurs most often in the labia minora and moist areas of the genital opening, vulva (external genitalia), anus (anus), It is found in the vagina and cervix (cervix) regions. In men, it is seen in the penis, urethra, scrotum, inguinal and rectal region. Warts may appear as soft, raised masses with a smooth (on the penile surface) or protruding (around the anus) surface. Although warts cause visual distress in people, they can also bring along complaints such as pain, bleeding and itching. These lesions should be treated because of the prevention of transmission to the sexual partner and the complaints they cause. 20% of people with genital warts also have other sexually transmitted diseases. Although warts cause visual distress in people, they can also bring along complaints such as pain, bleeding and itching. These lesions should be treated because of the prevention of transmission to the sexual partner and the complaints they cause. 20% of people with genital warts also have other sexually transmitted diseases. Although warts cause visual distress in people, they can also bring along complaints such as pain, bleeding and itching. These lesions should be treated because of the prevention of transmission to the sexual partner and the complaints they cause. 20% of people with genital warts also have other sexually transmitted diseases.
The presence of genital warts in children should raise suspicion of sexual abuse.
How to Treat Genital Warts?
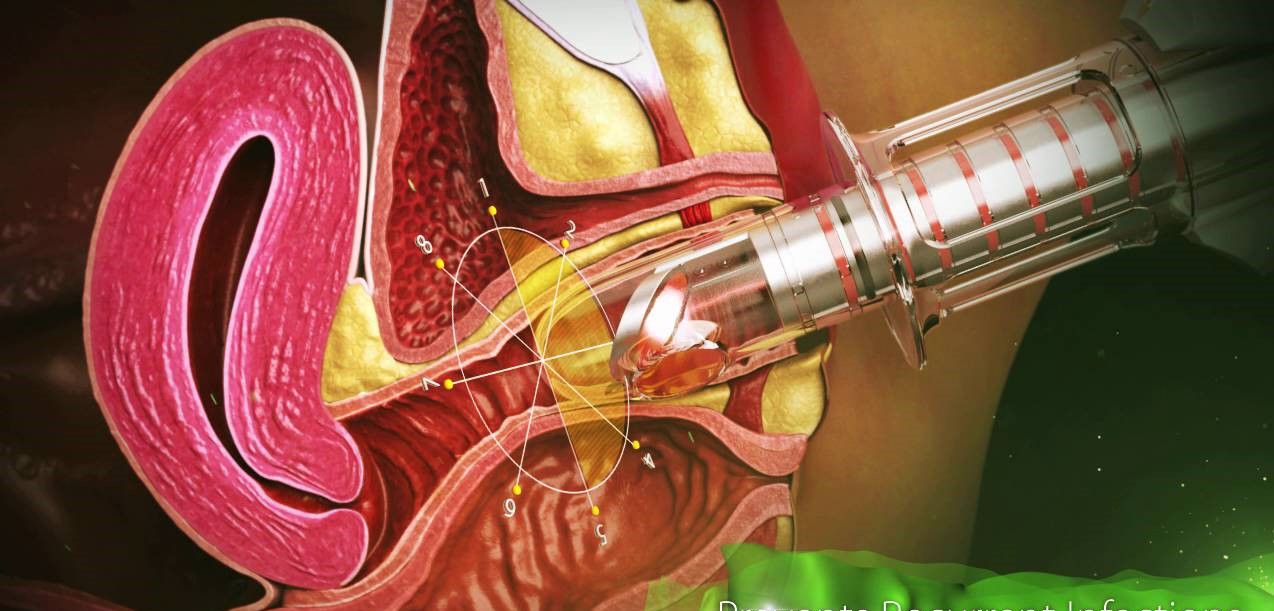
Surgical removal, Electrocauterization (burning), Cryotherapy (freezing), CO2 laser ablation, chemical destruction (bichloroacetic acid, trichloroacetic acid, podophylline, podophyllotoxin) can be applied to warts. However, treatment with cautery, burning of HPV foci, is the most valid treatment method accepted today. It is especially ideal for the removal of condylomas in the external genitalia. Generally, all foci can be destroyed in one go. The course of treatment is short. Chemical methods are substances that have an irritating effect on healthy skin, inflammation, erosion, pain and ulceration may occur. It is very difficult for the patient to apply it himself, if the healthy skin is touched, it will also cause damage here. It is also a long treatment option that requires repeated applications over several days.
Warts have the chance to recur in certain periods of life after burning, freezing and other treatments. The reason arises from the re-activation of the viral infection in case the body’s immune (immune) system drops from time to time for various reasons.
How to Protect from HPV?
HPV is transmitted through vaginal, anal or oral sex. Since HPV is transmitted through direct contact with the skin, HPV can be transmitted to partners from parts of the genitals that are not protected by condoms, or HPV can be infected. For this reason, the use of condoms in suspicious relationships cannot completely protect the person from HPV. HPV is not transmitted from toilet bowls, swimming pools, or the blood of a person with HPV. The only and surest way to prevent the risk of HPV infection is to not have sexual intercourse in any way, either vaginally, anal or orally. To reduce the risk of HPV transmission, monogamy and people with few or no sex partners should be selected. Gardasil (4-valent) and Gardasil (9-valent) vaccines protect against HPV. It is recommended to be done between the ages of 9-26. Gardasil-4 and Gardasil-9 vaccines are effective against HPV 6 and 11, which cause genital warts, It also provides protection against HPV 16 and 18, which are high-risk HPV types. focuses. Gardasil-9 also provides protection against high-risk HPV types 31, 33, 45, 52, 58.
Is There a Vaccine to Prevent Genital Warts? Who gets the HPV Vaccine?
In 2006, an HPV vaccine (Gardasil) was approved by the FDA. It is currently recommended for men and women ages 9 to 26. This vaccine has been shown to be safe and highly effective in preventing infection with the four most common HPV types (6, 11, 16, and 18) in women who have not been previously exposed to the virus. However, it is less effective in people already infected with HPV and does not protect against all types of HPV infection. Studies are ongoing to determine whether the vaccine is safe and effective in older women.
Gardasil 9 has activity against the four viral types in the basic Gardasil, but also has the 31, 33, 45, 52 and 58 virus types (for a total of 9 viral types). It’s also approved for men and women ages 9-26.
Cervarix is a bivalent vaccine developed against HPV types 16 and 18. It is approved by the FDA for women ages 10 to 25 but was withdrawn from the US market in 2016.
What are the Ways to Prevent Genital Warts?
Because no treatment is 100% effective, it’s important to prevent the spread of HPV, which causes genital warts and some cancers, whenever possible. The transmission of genital warts can be reduced by using a condom, and the infected individual should abstain from sexual activity until treatment.
Vaccination against HPV is recommended routinely for all girls from the age of 11. It is recommended up to age 26 as girls who are not yet sexually active are expected to benefit fully from vaccination. Although the overall vaccine efficacy may be lower when administered to sexually active women older than 26 years of age, it is thought that women in this age group will also benefit from vaccination at least partially. It is not applied to pregnant women, but since it is an inactive vaccine, it can be done during puerperium.
Gardasil Vaccine is administered intramuscularly in 3 doses. Even if vaccination is done, screening programs should be continued.
Is There a Diagnostic Test for Genital Warts and HPV?
The diagnosis is usually made from the appearance and appearance of genital warts.
In women, a colposcope can be used to look for lesions in the vaginal canal and on the cervix. A colposcopy is a magnifying instrument that magnifies the area to see lesions. Lesions can be seen with a technique called acetowhitening. This technique involves applying a 5% solution of acetic acid to the suspected area for about 5-10 minutes. Infected areas will turn white.
A routine Pap smear should always be done to look for HPV infection and abnormal cells in the cervix.
A biopsy may be done if the lesion appears unusual or recurs after treatment.
Special laboratory tests may also be used to confirm the presence of HPV infection.
What is the HPV Test?
The HPV test is a screening test for cervical cancer, but the test does not tell you if it is cancer. The HPV test detects the presence of genital warts, abnormal cervical cells, or human papillomavirus, a virus that can lead to the development of cervical cancer.
Your doctor may recommend HPV testing if your Pap smear is abnormal, shows unidentified atypical squamous cells (ASCUS), and you are 30 years of age or older.
HPV testing is only available for women; There is no HPV test yet to detect the virus in men. However, men can also be infected with HPV and pass the virus to their partners sexually.
Highly oncogenic types of HPV, including the most common types 16 and 18, increase your risk of cervical cancer.
Knowing whether you have a high oncogenic risk HPV type that causes cervical cancer risk means that you and your doctor can better decide on the next steps. These steps may require follow-up monitoring, further testing.
The routine use of HPV testing in women under 30 is not recommended. HPV is spread through sexual intercourse and is very common in young women, so often test results are positive. However, HPV infections can usually regress spontaneously within a year or two. Cervical changes that lead to cancer take several years (usually 10 years or more) to progress. Therefore, for cervical changes caused by HPV infection, careful follow-up can be followed instead of treatment.
What is the Difference Between Pap Smear Test and HPV Test?
A Pap smear test is used to detect cell changes or abnormal precancerous cells in the cervix. The cells are gently scraped from the cervix with a brush or spatula and sent to the pathology laboratory, where they are viewed under a microscope. The Pap smear test is a very good test to detect cancer cells and cells that may develop into cancer.
The HPV test detects the presence of the HPV virus, not cell changes. The HPV test can be done at the same time as the Pap smear test.
Can a Baby Get HPV During Birth?
If the mother has warts in her genital area, HPV can be transmitted to the baby’s mouth, throat and eye mucosa during normal delivery. When warts are seen in children under the age of 2, it is thought to be transmitted from the mother. Children over 2 years of age are considered sexual abuse.
The contact information of Jin.Op.Dr.Yeşim Yerçok (Gynecologist and Obstetrician ) for the treatment of condyloma (wart) caused by HPV is below:
For appointment Tel: 0216-3851715
Address: Fener Kalamış cad. Bullur apt. No:5 Da:9 Kiziltoprak/Istanbul